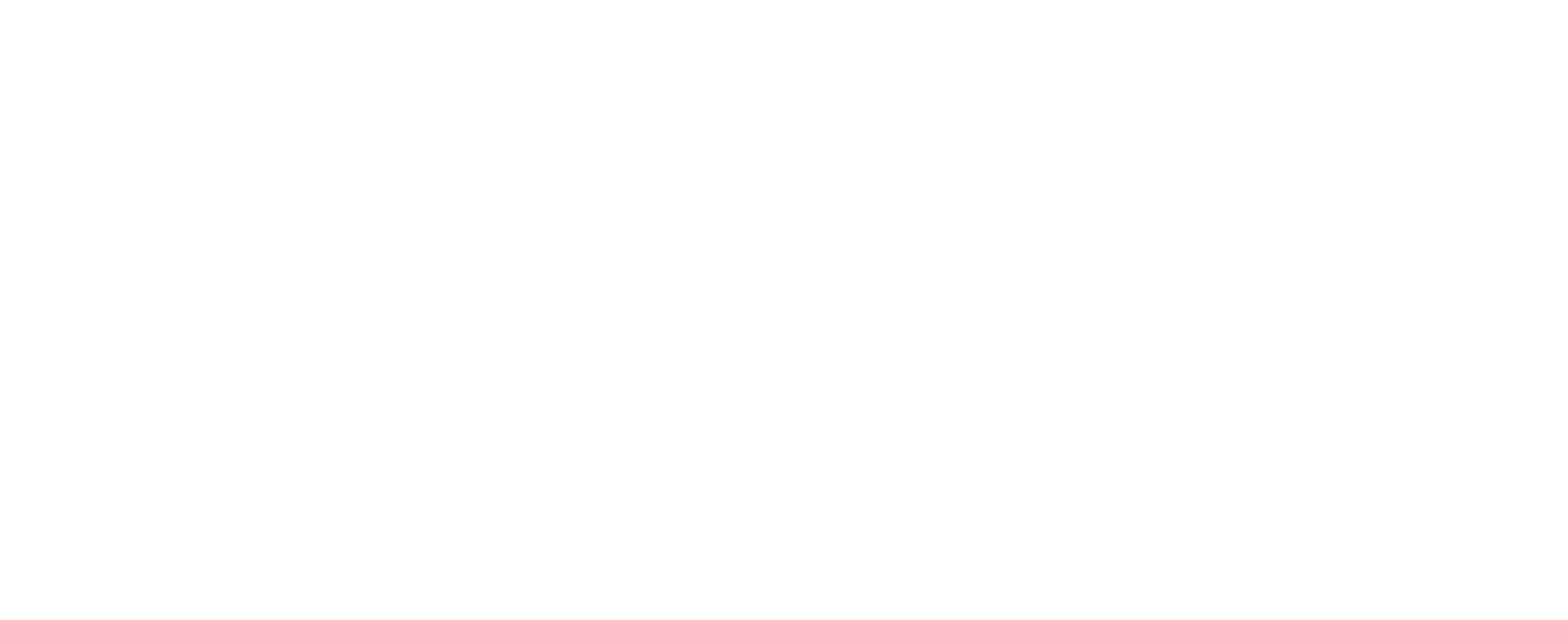
Musa Masala is happy to introduce Dr. Stephen Simon. Stephen is joining us as we launch our latest aid in our educational library. Here is the Musa Masala Heat Illness Card! As I write this it is 112 degrees F. outside, so what appropriate timing.
With people now getting outdoors during lockdown and our parks and wilderness areas seeing an increase in new visitors, we hope this article and our card will give you some straightforward information on how to protect yourself and others from an unwelcome experience. We will see rising temperatures as time goes on and being prepared for the future is an important part of our mission. Take the card whenever you are heading out into a hot environment. We recommend using it to go over your plan with your companions, too. Stay safe, stay healthy!
Thank you to Stephen Simon, who has taken the time out to help us. As a third year Emergency Medicine Resident at the Brooklyn Hospital, this has been a tough year with COVID-19, so we are very appreciative. When not working in the Emergency Department, Stephen can usually be found in his kitchen experimenting with new ways to eat bacon! An avid traveler, he tries to spend as much time as he can exploring the world with his fiancé, Lara, and their cat, Goopy.
Our Heat Illness cards are available at the Musa Masala store and, as with our altitude cards, we would love to customize each card with your company or organization’s logo. Contact us here.

5 Ways to Protect Yourself and Others Outdoors in Hot Weather
We know you’re cool (because you’re a fan of Musa Masala, duh!). But do you know how to stay cool? Heat-related illnesses are some of the most common medical emergencies that outdoor enthusiasts, athletes, and outdoors workers experience. Fortunately they are also entirely preventable, as long as you are prepared and know what to keep a lookout for. In this post, we will discuss a few important points about heat emergencies that will keep you safe, healthy, and cool as a cucumber.
1. Be prepared.
There’s a reason that the Boy Scouts made this rule number one, and you should too. Knowing the local conditions where you will be traveling is the first step toward knowing what to pack and what challenges you might face. You can spread out your drinks, food and emergency supplies between the group. In general, it is best to wear layered loose-fitting clothing, making sure to cover your head and using sunscreen on any exposed skin. Sunglasses are a must to protect your eyes from harmful UV light, even in the snow (tons of light gets reflected off the surface of the snow, more than enough to damage your eyes, often called snow blindness, and even give you a brutal sunburn!).
2. Find strength in numbers.
Make sure you share your plans with your friends and fellow travelers. Some signs of heat-related illness are subtle, and you may not notice these symptoms yourself. Having a friend keep an eye on you is a good way to recognize these signs early, and allow you to take some easy steps to remedy the situation before it becomes dangerous. Have a plan in case of an emergency.
3. Eat smart.
Having a properly fueled and well-hydrated body can make the difference between mild heat cramps and more severe conditions like heat stroke. Eating regularly will keep your blood sugar up, keeping you awake and alert. Low blood sugar can also mimic the signs and symptoms of heat illness. Be sure to avoid large amounts of caffeine, as it causes your blood vessels to constrict and limits your body’s ability to get rid of excess heat, and it is a mild diuretic. Most importantly, stay hydrated! (Read more on this below.)
4. Know the signs.
Recognizing a problem is the first step toward fixing it, and some of the heat emergencies we discuss here require different fixes, making it vitally important to know exactly what you are facing. It is always good to know if your traveling companions are diabetic, asthmatic or have any serious allergies or medical issues. Be sure to share yours with the group and give them the information they will need to help you if that becomes necessary. It is always important to take into account these possibilities when dealing with possible Heat illness.
Heat exhaustion
On the less severe end of the spectrum, you have Heat Exhaustion, Heat Cramps, and Heat Syncope. These three conditions comprise the first stage of heat illness. You may see only one of them, or you may see all three. The presentation varies, but generally involves headaches, dizziness, profound thirst, profuse sweating, slowing of pace or work, a low urine output and nausea/vomiting. Muscle cramps are the hallmark of Heat Cramps, while Heat Syncope may lead to fainting or light-headedness (also known as pre-syncope). These patients may have a fast pulse and be breathing quickly as their body tries to cool off. You can help by moving them to a cool place where they can rest and hydrate. They’re just worn out from the heat and exertion and need to rest. A lack of acclimation to a hot environment is a big factor in Heat Exhaustion. Take it slowly as you get used to being outside. Generally speaking, these conditions resolve in around an hour once the person has had a chance to cool off, replenish the water they’ve lost and snacked some while resting.
Heat stroke
If left unrecognized and untreated, the symptoms can progress to the next stage, known as Heat Stroke. This is a true medical emergency and must be evaluated in a hospital AFTER emergency cooling has taken place. Heat Stroke is the overwhelming loss of the body’s ability to regulate and dissipate heat leading to multi organ failure and eventual death. The defining feature of Heat Stroke is a change in mental status. This means that the temperature has become sufficiently high (> 40C) to cause confusion, hallucinations, or even seizures. If the person becomes overly agitated, aggressive, does not make sense or becomes unconscious, you need to move fast! Call for help immediately.
The most important initial step is to cool these patients quickly. If you can do so safely, immerse them in cold/ice water. Many race events will have children’s wading pools at the medical stations to allow them to immerse the patient with ice and cold water. If you have a tarp or a tent you can create a mini pool to cover your patient in the coldest water and ice available, circulating the water around the body. (Just to note, your patient will probably not be compliant and helpful, hopefully you will have assistance!) If this is not feasible, place ice packs into the creases of their body (knees, elbows, groin, armpits, etc…) The name of the game here is rapid cooling, do not delay this life-saving step.
It is possible for Heat Stroke to present without the signs and symptoms of Heat Exhaustion. It can come on quickly and be devastating. (This is why we stress that early recognition and prevention are the most powerful tools in your arsenal.)
Immediate cold-water immersion that brings down the body’s temperature to within normal limits has a great success rate. Conversely, not immediately cooling the patient has led to poor outcomes. A rectal thermometer reading is part of the standard for Heat Stroke diagnosing. We don’t expect you to carry one in the field so let’s look for a return to an alert and aware patient with the ability to converse and a heart rate and breathing that is within normal limits as a sign that your cooling is working. Then it’s off to the hospital.
5. Do not over-hydrate!
Finally, we must discuss the pitfalls of too much hydration (yes, there is such a thing) as it relates to a life-threatening condition known as Hyponatremia, aka water intoxication! In the backcountry, this is most commonly due to excessive water consumption, which dilutes the blood and disrupts the very delicate salt balance needed to support the metabolic functions of the body. Clinically this may be hard to distinguish from the other heat related emergencies. You may see headaches, nausea and vomiting, as with Heat Exhaustion or you may see confusion and seizures, as with Heat Stroke.
The one feature that should clue you into Hyponatremia is a history of excessive water consumption. (Importantly, this is why we emphasize the importance of the buddy system! Keeping an eye on your thirsty friend may help prevent him or her from over-hydrating and potentially developing Hyponatremia .) If you suspect Hyponatremia, you must call for help as this requires emergency medical care in a hospital. If the patient is awake and alert, you can consider giving them salty foods, but do not give them water (this will make things worse!). Marathon runners with Hyponatremia have actually gained weight through the race due to the amount of their water intake!

Treating Heat Illness in the time of COVID-19
While caring for someone with heat illness during the COVID-19 pandemic, here are a few suggestions that may help:
1. You still treat the patient for the signs and symptoms they present with. There are no changes in the treatment. Your approach however, must change.
2. If you do not already have a mask on, put one on. Make sure all who may be helping are wearing masks, too. Gloves and eye protection may be necessary in a case of Heat Stoke as the patient could be altered and combative. If your patient will tolerate a mask, put one on them as well.
3. If you take your patient into an enclosed room or car to cool off, know that your possibility for transmission increases. Try to maintain your physical distance, when possible.
4. Alert EMS or an emergency room if you have knowledge that your patient may be positive for COVID-19.

Heat illness represents a spectrum of conditions ranging from mild to life-threatening, and it is likely that trekkers will encounter some form of it over the course of their adventures. Prevention and early recognition are the two most important things that you can do to keep yourself and others healthy. We at Musa Masala hope that this knowledge inspires confidence and brings you peace of mind, allowing you to focus on the trail ahead.
Check out our Recommended Books section here for some excellent resources for information on heat related illness. Jam Jam!!