Now that you know the signs and symptoms of hypothermia, let’s discuss potential scenarios when hypothermia can set in and how you would manage it in the field. But first, let’s review different ways our body loses heat.
Heat Loss Modalities
There are 4 way the body loses heat:
- Conduction: heat loss by direct contact with something colder than your body temperature. Example: sitting on the cold ground
- Convection: heat loss due to moving air or water. Example: being exposed to high winds without appropriate clothing
- Evaporation: heat loss through evaporation of water from the skin and also through breathing. Example: having wet clothing on from sweating or from falling into a body of water
- Radiation: heat loss through infrared rays without physical contact.This happens whenever ambient temperature is lower than body temperature.
Being wet, undernourished, underdressed, injured and confused (from low blood sugar, head injury or alcohol intoxication) are the biggest risk factors to becoming hypothermic.

Now let’s put it all together and discuss management strategies based on how severe the hypothermia is.
Scenarios and Management
Mild hypothermia scenario:
Your friend just capsized her kayak and fell into the lake. It’s a warm September day, 75°F, in the New York Adirondacks. You help her get to the shore and notice that she is trembling, but otherwise alert. She sits down on the rock and continues shivering.
You suspect that she is suffering from mild hypothermia (and likely some anxiety!) given that she is alert and shivering. You also notice that she does not exhibit the best judgement at the moment. Instead of getting inside her tent and putting warm clothing on, she is sitting exposed on the rock mumbling, thus continuing to lose heat.
Your management strategies for mild hypothermia include:
- Do not leave the hypothermic person alone as they might have poor judgement and not be able to take care of themselves. (Poor judgement and poor self-care are specific signs to look for, Cold Stress is a similar condition, but your patient is still alert and functional). A cold stress patient may still move around to warm up, but an altered hypothermia patient may not.
- Get them into shelter (out of cold and wind) or at least have them sit on something insulating (i.e. a sleeping pad or backpack) to prevent conductive heat loss.
- Remove wet clothing (only if there is a shelter) and replace it with dry clothing on to stop evaporative heat loss.
- Initiate passive warming by giving them a high-calorie drink or food (hot cocoa is a great choice) so they can continue to generate heat by shivering.
- Once heat loss has stopped, don’t allow walking or standing for 30 minutes. They can continue their outdoor adventures when they are back to baseline. Baseline is an alert, oriented patient who is functioning normally.
Moderate hypothermia scenario:
You are out skiing tree runs with a friend and notice a red jacket at the bottom of a large boulder. When you move closer, you notice a young man who keeps meekly repeating that his leg is broken. You can’t get much else out of him. He has a deformed lower leg with his ski boot still on. He is not moving much. You think that he broke his leg and might have spent the whole night lying in the snow.
Given his depressed mental status and lack of shivering, you suspect that he is suffering from moderate hypothermia. Although he’s wearing a helmet, you are not sure if he might have an internal head injury as well.
Your management strategies for moderate hypothermia include:
- Treat other life-threatening conditions first (severe hemorrhage, airway obstruction, etc.).
- Call for help. Call the ski patrol or send your friend down with the exact location to get help.
- Handle gently. Remember, hypothermic patients are prone to getting fatal arrhythmias that can be provoked by even subtle movement.
- Move off the cold ground and provide shelter/covering to minimize further heat loss. In this case, place branches or your backpack under the patient. If you have an extra layer with you, give it to the patient. If you see a good natural shelter close by that will keep the patient out of the wind, you can move him there. Only move the patient if you are not concerned for a spinal injury or if you can move him while keeping his spine protected.
- Active warming: apply heat to the upper torso such as heat packs or bottles with warm water to warm the core. Do not place the heat packs directly on the skin to avoid thermal burns. More advanced treatment includes administering warmed intravenous fluids and intravenous glucose.
- Consider giving oral glucose gel (place inside the cheek) if you have one if there is a delay in getting professional help.
- Patients with moderate hypothermia need to stay prone and will require evacuation to the nearest hospital to continue active rewarming. In the above case, the patient also needs to be assessed for trauma.
Severe/profound hypothermia scenario:
You are in Tanzania attempting a Mt. Kilimanjaro ascent. It’s day 4 out of 7 and you are at 4,000 meters (13,000 ft). You just finished dinner and walked away from the camp to check out the Milky Way when you stumble across a middle-aged man in his underwear lying in the snow.
You approach him and notice that he is not moving, other than having occasional chest rise. He does not respond to you shouting at him or you pinching his skin. It takes you almost a minute to feel his pulse. There are no obvious injuries.
You are concerned that he has severe hypothermia given his slow heart rate and nonexistent mental status. Given the high altitude, high altitude cerebral edema (HACE) is also of high concern.
Your management strategies for severe/profound hypothermia include:
- Handle gently to avoid precipitating a fatal arrhythmia.
- Call for help as this patient will require advanced medical care.
- Move them from the snow into shelter to avoid further heat loss.
- Initiate active warming by applying heat to the upper torso (heat packs, warm water bottles).
- Give oxygen if at high altitude (above2,500m). Your guide happens to have some.
- Consider giving them glucose gel if there is delay in getting professional help.
- Treat the underlying cause—in this case, suspected HACE. (Treatment is that oxygen and descent!)
- If this patient deteriorates and you no longer can feel the pulse, initiate chest compressions. A patient who suffers cardiac arrest due to severe hypothermia, has a high chance of making a full neurological recovery if they receive quality CPR and are aggressively rewarmed.
- Patients with severe hypothermia or with cardiac arrest from hypothermia need to be emergently evacuated to receive further medical care. This includes advanced airway management, more aggressive rewarming strategies and cardiopulmonary support. In this case, a helicopter with night vision capabilities would be required to get this patient quickly to a hospital.
You might wonder why this person was found in his underwear if he was getting cold. This is a common phenomenon seen in people with more advanced hypothermia termed “paradoxical undressing.” There are two different theories as to why this occurs.
One, the brain loses its ability to thermoregulate once the temperature crosses a certain threshold. Two, the vessels in the extremities “give out” and relax causing the warmer blood from the core to flow toward the extremities, making the person feel flushed and warm, thus causing them to undress. If you see someone undressed and confused in the cold environment, beware, they probably need help.
Avoiding hypothermia
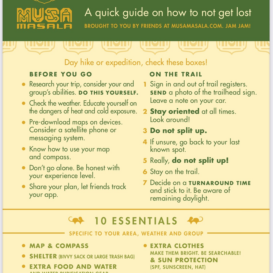
Hypothermia is a serious condition and can be deadly. The best thing you can do is to avoid it is by following the Musa guidelines to:
1. PLAN AHEAD (Know your limits.)
2. INVEST IN AND BRING THE RIGHT GEAR.
3. STAY HYDRATED AND WELL-NOURISHED.
The next best thing is to be able to recognize it early and treat it so that it does not progress. Recognizing more advanced hypothermia can help you initiate immediate treatment and emergent evacuation. Always consider other dangerous conditions (head injury, high altitude cerebral edema, etc.) that can coexist with or mimic hypothermia.
STOP. PLAN. GO.
Stop the activity.
Plan your actions.
Go act out your plan with purpose!
Stay warm and safe out there!



You and two friends come upon this skier. What would your plan be? Do you think this person needs medical help? Why? Email us at info@musamasala.com with your plan.The best answer wins a valuable prize! We will share the answers and announce the winner in our next post. Jam Jam!!
Thanks to Addi Stunts for the scenerio realism!